By arhospice on April 22nd, 2019

By Brian Bell, M.D.
“You matter because you are you, and you matter to the end of your life. We will do all we can not only to help you die peacefully, but also to live until you die.” This quote from Dame Cicely Saunders, the founder of the modern hospice movement, is not only applicable to hospice but rings true for hospitals as well. Despite the majority of people wishing to die at home, many deaths still occur in hospitals. In this regard, hospitals have the opportunity, as well as an obligation, to work with hospice programs to provide optimal end-of-life care for patients with serious and life-threatening illness. As a hospice physician, I constantly hear from the families of patients the sentiment of wishing they had enrolled their loved one into hospice care sooner. It translates not only to better care for the patient, but also can benefit hospitals with improved quality scores, staff utilization, and lower costs per patient.
Hospice is a specialized program that provides symptom management and comfort care for patients with a life expectancy of six months or less. Care encompasses meeting the physical, psychosocial, emotional, and spiritual needs for patients and their families. The interdisciplinary hospice care team consists of physicians, nurses, hospice aides, social workers, chaplains, bereavement specialists, and volunteers who contribute to each patient’s individual care plan. Hospice care can be provided in any care setting. In the hospital, it is often provided through the general inpatient (GIP) level of care for patients who have uncontrolled symptoms.
Benefits of a Hospital and Hospice Collaboration:
For the Hospital:
- Improve and streamline post-acute care transitions
- Decrease LOS by transitioning hospice-eligible patients to appropriate venues of care
- Improved Value Based Purchasing scores with decrease in 30 day readmissions, CAHPS and Medicare Spending per Beneficiary
- For hospital with ACO/CIN: decrease utilization and achieve cost savings
- New stream of income for patients transitioned to GIP within the hospital
- Education of staff on end-of-life care
- Access to bereavement services for families of mutual patients provided by hospice provider at no cost to hospital
For the Hospice:
- Access to more patients who will benefit from hospice care
- Venue to provide GIP level of care
- Educate hospital staff on the holistic approach of hospice and palliative care
- Gain access to the hospital’s resources and create further partnerships within the health system
- Understand the unique challenges of acute care hospitals
- More timely and appropriate hospice referrals through improved integration
- Establish or participate in development of hospital-based palliative care programs
Improved quality scores for hospitals
As noted in the preceding chart, hospices and hospitals can have a mutually beneficial relationship. This is primarily achieved by hospitals and hospices working together to provide expert care for patients approaching their life’s end. This quality is demonstrated by better pain and symptom control and improved communication, which may be reflected in CAHPS scores for not only the hospice, but the hospital, as well. An article titled “30-Day Readmissions among Seriously Ill Older Adults” published in the 2012 Journal of Palliative Medicine indicated that patients who received a palliative care consult and were discharged with a hospice provider had significantly lower 30-day readmission rates compared to other discharge scenarios. (1)

The results have been even more pronounced in Arkansas. In 2015, Medicare beneficiaries who were discharged from the hospital with hospice only hada 1.3% 30-day readmission rate.
Transitioning patients efficiently to a post acute venue is important for hospitals to decrease length of stay. Most hospices admit patients 7 days a week, and within hours of the admission decision, if appropriate arrangements can be made to safely care for a patient at his/her preferred location. This streamlined discharge process can not only benefit patients, but make case management’s job much easier. Through integration of hospice in the acute care hospital, both groups can gain a better understanding of the rewards and challenges of the other provider.
The hospital case manager’s job can be made much easier through appropriate discharge arrangements from the hospital to a hospice care provider.
This collaboration can serve as a catalyst for enhanced communication, greater respect for each other’s contributions, and serve to provide superior patient and family-centered care.
Cost reductions for hospitals
Another 2012 study published in the Journal of Palliative Medicine indicated that adult patients admitted to two western New York hospitals clearly displayed lower cost per admission among patients discharged with hospice care. On average, the cost per admission was $1,401 less (13% lower) than comparison patients, also accompanied by “significantly lower” readmission rates. (2) Additionally compelling is a 2013 Health Affairs article that indicated patients who were enrolled in hospice for 53 -105 days compared to a matched cohort, showed a cost savings of $2,561 to Medicare. Additionally, the article revealed these hospice patients also had “fewer hospital admissions, intensive care unit admissions, hospital days, intensive care unit days, thirty-day hospital readmissions, and in-hospital deaths.” (3)
Patient satisfaction
According to Medicare’s Hospice Compare website, regardless of whether patients are in the hospital or their home, hospice patients and their families are very satisfied with the care they receive. Nationally, 96% of families who have had loved ones die in hospice would “probably or definitely” recommend hospice to others. (4) Ratings for individual hospices in Arkansas can be found online at www.medicare.gov/hospicecompare.
Increased census for hospice providers
Hospitals traditionally have been a major referral base for hospices. One of the main collaborations that occur is when a hospice either contracts or leases space within an acute care hospital, since 23% of patients die in a hospice general inpatient setting. (5) With a closer strategic partnership, hospice providers hope to gain access to patients that would benefit from those services, and most importantly, in a more timely fashion.
In 2015, the median length of stay (LOS) for a hospice patient nationwide was 23 days, with 28% of these patients in hospice less than 7 days. (5) These short LOS’s do not create the proper therapeutic environment to meet all the needs of patients and their families.
Utilization of hospice care
Nationally, the number of Medicare beneficiaries receiving hospice services has grown from 513,000 in FY 2000 to nearly 1.4 million in FY 2016. Similarly, Medicare hospice expenditures have risen from $2.8 billion in FY 2000 to approximately $16.5 billion in FY 2016. (5)
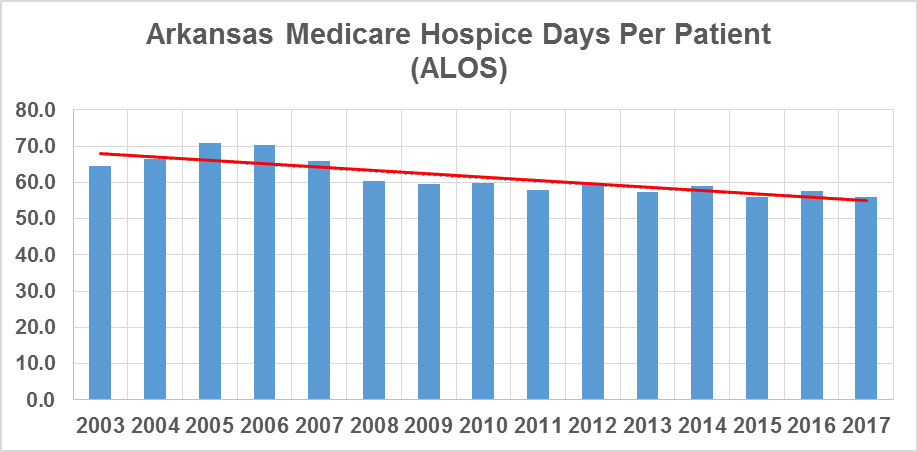
Among Arkansas Medicare recipients, hospice census has significantly increased in recent years. From 2003 to 2017, enrollment for hospice care in the state has grown 34.9% (from 475,705 to 641,190) while the number of GIP hospice patients served over the same period has grown 527.2% (from 970 to 5,114). Initially, this appears as good news, showing more patients receiving hospice care. However, other indicators point toward patients being admitted into hospice at later stages of disease, therefore negating the benefits of comfort care to patients and supportive care for families that require weeks – not days – to fully benefit from a hospice plan of care. For example, the average length of stay (ALOS) in hospice was 64.6 in 2003, peaked at 70.7 in 2005, but has steadily declined to 56 in 2017.
Bringing it all together
Hospitals in Arkansas have the opportunity to work with hospice care providers in their area. It is crucial for hospitals and hospice care providers to take a team approach to ensure we achieve the Triple Aim: better outcomes, improved patient experiences, and lower costs. Most importantly, hospitals and hospices have the duty to all Arkansans to provide the best end-of-life care possible. When we achieve that, we all win.
- Susan Enguidanos, Evie Vesper, and Karl Lorenz. 2012 “30-Day Readmissions among Seriously Ill Older Adults” Journal of Palliative Medicine. Volume 15, Number 12 1356-1361
- John C. Tangeman, MD, FACP, Carole B. Ruda, PhD, MPH, Christopher W. Kerr, PhD, and Pei C. Grant, PhD. 2014 “A Hospice-Hospital Partnership: Reducing Hospitalization Costs and 30-Day Readmissions among Seriously Ill Adults” Journal of Palliative Medicine. Volume 17, Number 9 1005-1010
- Amy S. Kelley, Partha Deb, Qingling Du, Melissa D. Aldridge Carson, and R. Sean Morrison. 2013 “Hospice Enrollment Saves Money For Medicare And Improves Care Quality Across A Number Of Different Lengths-Of-Stay” Health Affairs. Volume 32, Number 3 552–561
- https://data.medicare.gov/data/hospice-compare
- NHPCO Facts and Figures: Hospice Care in America. Alexandria, VA
National Hospice and Palliative Care Organization, Rev. ed. April 2018
About the author:
Dr. Brian Bell is a native of Little Rock and a graduate of the University of Arkansas for Medical Sciences. He is Board Certified in Family Medicine and Hospice and Palliative Medicine, and has worked in hospice since 2006. He was previously the Palliative Care Medical Director for Spartanburg Regional Medical Center in Spartanburg, South Carolina. He also started the first Palliative Medicine Fellowship program in South Carolina and served as its Program Director. He is currently Vice President and Chief Medical Officer of Arkansas Hospice.
This article first appeared in the Spring 2019 edition of Arkansas Hospitals magazine, a publication of the Arkansas Hospital Association. Used with permission.


 Registered 501(c)(3). EIN:
Registered 501(c)(3). EIN: